Technologies in Emergency Care - TEC Vancouver Conference 2019
Jump To: Conference Overview & Brochure | Registration | Speakers & Content | FOAM Bar | About the Organizers | Sponsors | Connect with Us
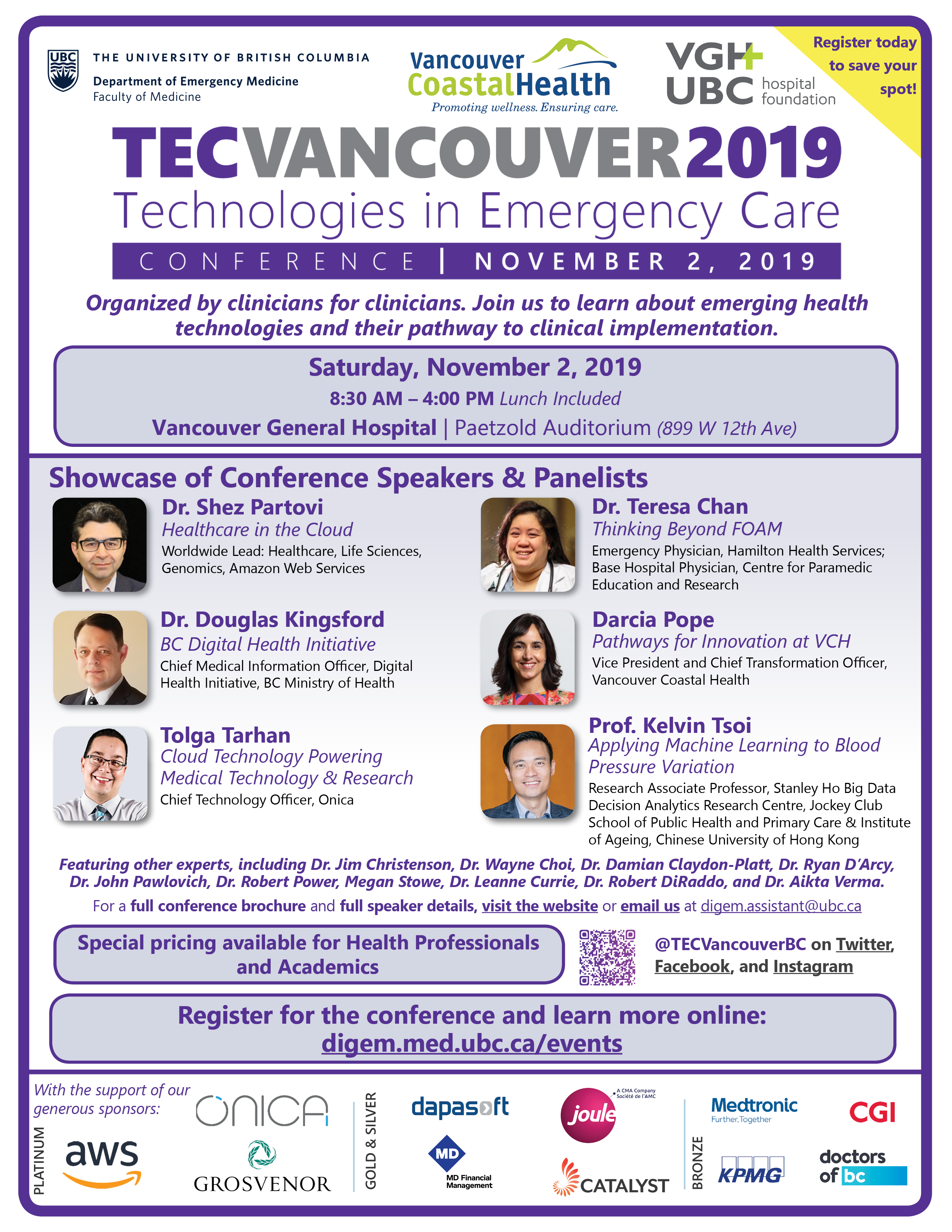
Organized by clinicians for clinicians, TEC Vancouver brings health professionals, health organizational and industry leaders together to apply innovations to real life challenges in primary and emergency patient care in BC and beyond.
Top reasons to be at this conference:
- See how health professionals apply innovations for patient care and education
- Hear emerging trends of digital health from international clinician leaders, health policy leaders and industry experts
- Participate in dialogues on healthcare gaps seeking technology solutions
- Network with like-minded colleagues to generate ideas and pathfinding approaches
Registration for TEC Vancouver 2019 is now closed. Save the date for the next TEC Vancouver conference - Saturday, May 15, 2021! More details: https://ubccpd.ca/tec2021
For further information about what was covered at TEC Vancouver 2019, please see the following documents and media:
Follow us @TECVancouverBC on Twitter, Facebook, and Instagram to stay up-to-date!
Conference Overview
| Date: | Saturday, November 2, 2019 | |
| Time: | 8:30 am to 4:00 pm PST | |
| Venue: | Vancouver General Hospital Paetzold Auditorium 899 W 12th Ave Vancouver, BC V5Z 1M9 |
Conference Registration
Are you interested in joining us to learn about emerging health technologies and their pathway to implementation? Continue reading for more information about registration for TEC Vancouver 2019.
TEC Vancouver welcomes health professionals, health administrators, and health professional trainees to register. There will be a variety of programming aimed at professionals interested in gaining deep, diverse exposure to the latest topics involving technology in emergency and primary care.
Conference registration is open to:
- Allied Health Professionals
- Health Administrators & Policy Makers
- Health Professional Trainees
Industry leaders interested in participating are invited to contact digem.assistant@ubc.ca for corporate involvement.
In addition to enjoying a comprehensive day of programming including lectures, question & answer periods, and panel discussions, your registration to TEC Vancouver includes several perks.
- Networking opportunities with both up-and-coming and established leaders in the field of health technology
- Complimentary catered lunch and refreshments throughout the day
- A certificate of attendance (upon request)
TEC Vancouver is excited to offer discounted pricing for non-clinical academics, nurses, residents, medical students, and allied health professionals. Please see full pricing details below.
| Admission Fee | |
|---|---|
| General Admission | |
| Non-Clinical Academics | |
| Reduced Rate* |
For group purchases, please contact digem.assistant@ubc.ca.
*The reduced rate applies to nurses, residents, medical students and allied health professionals. Please provide proof of your status at our registration desk during check-in on the conference day. A certificate of attendance can be provided upon request.
Registration for TEC Vancouver 2019 is now closed. Save the date for the next TEC Vancouver conference - Saturday, May 15, 2021! More details: https://ubccpd.ca/tec2021
Speakers & Content
We are excited to present the speakers & panelists for TEC Vancouver 2019. Click below to see their biographies and the details of the talks. A detailed schedule is available in the conference agenda.
Keynote Speakers
 Dr. Shez Partovi, MD
Dr. Shez Partovi, MD
Worldwide Lead, Healthcare, Life Sciences, Genomics, Amazon Web Services
The path to precision health is dependent on both precision diagnostics and precision therapeutics. In this presentation we will review how different peer organizations have embarked on the journey of precision medicine by leveraging the power of Amazon Web Services.
Dr. Shez Partovi obtained his medical degree from McGill University and completed his neuroradiology subspecialty training at Barrow Neurological Institute. His undergraduate program at UBC was in Life Sciences and Computer Science. He is a serial entrepreneur and has launched a number of health IT companies. After a decade of clinical practice, Dr. Partovi transitioned into an executive role at the 4th largest health system in the US, where he served as its Chief Digital Officer/SVP of Digital Transformation. Dr. Partovi joined Amazon Web Services in 2018 as the Worldwide Lead for Healthcare, Life Sciences and Genomics.
 Professor Kelvin Tsoi, BSc PhD
Professor Kelvin Tsoi, BSc PhD
Research Associate Professor, Stanley Ho Big Data Decision Research Centre
Associate Professor, Jockey Club School of Public Health and Primary Care, and Jockey Club Institute of Ageing, Chinese University of Hong Kong
Professor Tsoi's talk will give insight on how Digital Health reduce the burden of health system by applying machine learning techniques on the blood pressure variation to predict the risk of hospitalization among hypertensive patients.
Professor Kelvin Tsoi is a Digital Epidemiologist and Data Scientist. He is the President of the International Society of Digital Health. His Doctoral degree in Medical Sciences and Bachelor degree in Statistics were obtained from the Chinese University of Hong Kong. His research focuses on Digital Health, including data capturing techniques, machine learning application and sensor data with wearable devices. Professor Tsoi is currently conducting research on the non-communicable diseases in ageing population with digital dementia screening and machine learning on blood pressure variability.
Invited Speakers
 Dr. Wayne Choi, MD FRCPC
Dr. Wayne Choi, MD FRCPC
Emergency Physician, Royal Columbian Hospital
Member of the Board, Section of Emergency Medicine, Doctors of BC
A patient’s emergency department (ED) visit is often very stressful: Why am I waiting so long? What happens during the visit? What do I need to know after I’m discharged? Dr. Choi will discuss how he and his team are striving to improve the patient’s experience via an app.
Dr. Wayne Choi is a full time Emergency Physician at the Royal Columbian Hospital. Prior to medicine, he worked in the software industry with a focus on user experience. Now, Wayne combines his skillset in both, holding a special interest in the intersection of technology, innovation, and medicine. He has designed an ultrasound logging app for education, EchoLog, used across the country. He is also on the board of the Section of Emergency Medicine of Doctors of BC.
Presenters
Kathy Steegstra, BScN BEd MEd
Senior Provincial Executive Director, Office of Virtual Health, Trauma Services, BC Provincial Health Services Authority
Using technology to improve health care delivery in B.C.
Background Virtual Health is a patient-centred care model focused on connecting patients, families and providers, using technology to optimize wellness, specialty care and outcomes. A 2017 Provincial Health Services Authority (PHSA) survey (We are listening) identified that patients and their families were asking for Virtual Health solutions to improve their access to care. That same year, the mandate letter from B.C. Ministry of Health to PHSA specified that virtual care be leveraged and enhanced as part of the care continuum. The Office of Virtual Health (OVH) was created shortly after, with an ambition to support people to receive treatment and stay well by connecting them to care, seamlessly, when and where they need it. Current status - Strategic engagement with PHSA clinical programs helped determine our clinical priorities.
We are currently working on four clinical priorities: 1. Anywhere to anywhere 2. Remote patient monitoring 3. Online therapy 4. Clinical digital messaging With patients as our partners, we are focused on improving patient and family outcomes and experience. Patients are involved every step of the way, from identification of the clinical need, to the selection of new solutions, evaluation and future planning.
The OVH has engaged patients and clinicians in testing various technical solutions, called demonstration projects. Our project lifecycle includes six stages: 1. Engagement 2. Discovery 3. Planning 4. Execution 5. Evaluation 6. Scale Currently 19 clinical programs are participating in various stages of demonstration projects, using one of nine technical solutions. Conclusion Our work addresses the need to improve care delivery for both patients and providers. OVH is leading a system-wide transformation that will see Virtual Health integrated into clinical services as one system of care offering a set of effective and efficient patient-centred solutions that respond to the digital world we live in.
Dr. Kendall Ho, MD FRCPC
Professor, Faculty of Medicine, The University of British Columbia
Lead, Digital Emergency Medicine, Faculty of Medicine, The University of British Columbia
Spencer: Home monitoring of medications to improve adherence and reduce adverse events
Seniors taking multiple medications at home can be challenging for the patients, their caregivers, and their health professionals. Due to polypharmacy, patients can easily get confused regarding frequencies and timing of different medications. Even though there are instruments like bubble packing of medications, or clinicians calling patients or even observing them in medication intake, these isolated solutions can be time consuming for health professionals, inconvenient for patients, or only partially addressing the problems.
Spencer, the integration of packaging of patients’ medications, together with a convenient digital dispensing of them at home to facilitate intake, coupled with capabilities of the unit to connect with health professionals remotely for monitoring and responding to queries, is conceivably a very useful platform. Pharmacists, nurses, and physicians can work together to remotely monitor patients for correct time and dosing, while patients and caregivers have the security to know that they have the right dosing and also seek help whenever necessary at the comfort of their homes. This approach is being studied in BC to validate its utility, and how it can help primary health professional teams to support patients and caregivers for optimal medication management at home.
Jeffrey Hau, MSc
Research Coordinator, ActionADE, Centre for Clinical Epidemiology and Evaluation, Vancouver Coastal Health
Serena Small, MA
Research Coordinator, ActionADE, Centre for Clinical Epidemiology and Evaluation, Vancouver Coastal Health
Implementing and Evaluating ActionADE to Transform Medication Safety
Adverse drug events (ADEs), unintended and harmful events resulting from medication use, cause over 276,000 emergency department visits, 100,000 admissions, and 4,500 deaths annually in British Columbia (BC). Patients are commonly reexposed to medications that previously caused harm, which can result in repeat ADEs. Ineffective processes related to the documentation and communication of ADEs among clinicians in a patient’s circle of care is a substantial contributing factor.
In response to this gap, our research team has developed a software application called ActionADE that enables frontline clinicians to document ADEs in a user-friendly and standardized manner. We developed ActionADE using a participatory design process that engaged clinician end-users throughout the design, piloting, and refinement process. We have partnered with the BC Ministry of Health, Vancouver Coastal Health, Lower Mainland Pharmacy Services and the College of Pharmacists of BC to pilot the integration ActionADE with PharmaNet, BC’s medication dispensing database, using a minimum viable product. This will enable the transmission of ADE information from participating hospitals to a central repository that will be accessible to other clinicians in the patient’s circle of care. With integration, ADE data entered in ActionADE will generate alerts if community pharmacists attempt to re-dispense medications that previously caused harm.
We will evaluate whether ActionADE achieves its goals of preventing re-exposures to harmful medications, and improving patient and health system outcomes in a randomized controlled trial. We will complete an economic evaluation to examine ActionADE’s incremental costs and benefits compared to standard care. ActionADE has the potential to enhance patient care, improving population health, improving health system sustainability, and supporting the work of clinicians. If beneficial, ActionADE may inform future developments of PharmaNet, and systems to facilitate ADE reporting and communication in other health sectors, including in hospitals, long-term care facilities, and physician offices to transform medication safety.
 Dr. Douglas Kingsford, BHB MBChB PhD FRNZCGP
Dr. Douglas Kingsford, BHB MBChB PhD FRNZCGP
Chief Medical Information Officer, Digital Health Initiative, BC Ministry of Health
Driven by a need and opportunities to improve quality of care, improve population health, increase access to care, provide better patient and clinician experience, and improve clinician productivity and overall system efficiency, the Ministry of Health has launched the provincial Digital Health Initiative. Dr. Kingsford will present the DHI and its implications for care delivery.
Dr Kingsford is Chief Medical Information Officer of the Provincial Digital Health Initiative with the Ministry of Health and co-chair of the Information Privacy and Security Standing Committee. He is a primary care physician with an Electronic Engineering PhD in artificial intelligence, with particular interests in artificial intelligence, machine learning, interoperability, integrated care and workflow coordination.
 Tolga Tarhan, MBA
Tolga Tarhan, MBA
Chief Technology Officer, Onica
The cloud is changing how the world innovates. In this talk, Tolga will explore how the cloud is powering the next generation of medical devices and research.
As Onica’s Chief Technology Officer, Tolga Tarhan leads the company’s technological vision by pushing innovation and driving strategy for product development and service offerings. With two decades of experience leading and hands-on software development, his cross-functional technical expertise gives him unique insight into the best approaches for building complex systems and applications. Tolga has an MBA from Pepperdine University and helps customers strategize beyond technology solutions to improve their businesses and grow their bottom line.
Invited Speakers
 Dr. Jim Christenson, MD FRCPC
Dr. Jim Christenson, MD FRCPC
Professor and Head, Department of Emergency Medicine, University of British Columbia Faculty of Medicine
Executive Lead, BC Emergency Medicine Network
During this presentation, Dr. Christensen will discuss the BC Emergency Medicine Network and its impact on Emergency Medicine in BC.
Dr. Jim Christenson is an emergency physician at St. Paul’s Hospital in Vancouver. He is a Professor and Head of the Academic Department of Emergency Medicine at the University of British Columbia. He has a wide range of experience in emergency care clinical research, related to clinical decision rules and resuscitation.
Dr. Christenson leads a team that built and launched the BC Emergency Medicine Network (EMN) to facilitate knowledge sharing and clinical support for all emergency practitioners in British Columbia. It is growing quickly and utilizing technology to change the way emergency care providers in all emergency settings are supported and how they communicate new knowledge and practice change.
Presenters
Andrew Tan
Researcher
Samarth Shyamanur
Researcher
Vicky Wang, BCom
Researcher
Redirecting Non-Urgent Emergency Department Patients To Alternative Healthcare Facilities
Overcrowding of emergency departments (ED) is a significant problem in the Canadian public healthcare system. According to the Canadian Institute for Health Information (CIHI), the median emergency room wait time to see a physician is 2.7 hours. Individuals with non-urgent conditions are turning to emergency rooms instead of going to a non-emergency facility such as a walk-in clinic. Hospital resources become overutilized and staff become overburdened, with non-urgent individuals also forced to wait exceedingly long times to be treated due to their low priority assessment (Canadian Triage and Acuity Scale Level 4, 5).
A potential solution to this problem is a software that allows triage staff at hospitals to redirect non-urgent patients to less crowded walk-in clinics nearby. Thus, the number of non-urgent patients in EDs will decrease, the number of patients at clinics will increase and the overall wait time for patients will be reduced. The research was formed with consultation with over 24 medical professionals, including hospital directors, such as Dr. Heather Lindsay (Department Head and Medical Director of Emergency Medicine at Vancouver General Hospital), physicians, nursing and representatives from Vancouver Coastal Health and Providence Health Care, clinics, and healthcare software providers. Furthermore, we surveyed 76 potential patients, with 83% willing to divert to the nearby walk-in clinics for a faster time to physician, given their nonurgent triage status.
Applying this research results in system-wide cost and resource savings. British Columbia’s Medical Services Plan (MSP) indicates a physician at a hospital ED bills 4 times as much as a physician at a walk-in clinic for the same patient with the non-urgent condition. Hospital EDs can use resources more effectively and reduce stress on staff, and clinics can increase their utilization rates. Ultimately, patients have better care as a result of transparency and awareness in their healthcare.
Jaime Gallaher, RN MSN
Regional Educator, Vancouver Coastal Health
Michelle Connell, RN MSN
Simulation Educator, Coastal Simulation Team, Vancouver Coastal Health
Technology Enhanced Healthcare Simulation
Technology Enhanced Healthcare Simulation is an educational tool with which the learner physically interacts to mimic an aspect of clinical care for the purpose of teaching or assessment (INACSL, 2019). Within British Columbia, multiple centers are using simulation in their emergency departments for the purpose of teaching and team building to improve patient outcomes and decrease departmental latent safety threats. Latent safety threats are defined as errors in design, organization, training or maintenance that may contribute to medical errors and have a significant impact on patient safety (Wetzel et al, 2013).
Within Vancouver Coastal Health (VCH) a unique method of delivery for these in situ simulations is being used to facilitate emergency department critical care situations in rural sites via telehealth technology called “telesimulation.” Telesimulation consists of blending simulation technology platforms with telehealth monitors and audio capabilities to help conduct and facilitate emergency department simulations to those in hard to reach geographical areas. This talk will discuss the emerging role of telesimulation in the simulation landscape here at VCH.
 Dr. Teresa Chan, HBSc BEd MD FRCPC MHPE DRCPSC
Dr. Teresa Chan, HBSc BEd MD FRCPC MHPE DRCPSC
Emergency Physician, Hamilton Health Sciences
Base Hospital Physician, Centre for Paramedic Education and Research
Assistant Professor, McMaster University
Dr. Chan will discuss the ins and outs of the current models for operating FOAM organizations and reveal some of the systemic threats, and invite participants to consider how online continuing education will evolve in the coming years.
Dr. Teresa Chan is an assistant professor at McMaster University. Locally, she is the Specialty Committee Chair of the RCPSC Clinician Educator Area of Focused Competency Diploma program, and the McMaster Program Director. Dr. Chan is one of the founding members of the CanadiEM website, the MedEdLIFE research collaborative, and a key member of the METRIQ Study Group. She is the Chief Academic Officer of the international Faculty Incubator program for the Academic Life in Emergency Medicine (ALiEM) group. Dr. Chan is also interested in developing & evaluating medical education innovations.
 Dr. Robert DiRaddo, PhD
Dr. Robert DiRaddo, PhD
Chief Medical Information Officer, Digital Health Initiative, BC Ministry of Health
Robert will present his group’s current research work in digital therapeutics and digital monitoring, with particular emphasis on projects with the B.C. ecosystem and work of relevance to emergency medicine.
Robert DiRaddo obtained his PhD in Engineering from McGill University in Montreal. He started his career in the private sector working at two multi-national companies. He then moved to the NRC starting as an Assistant Research Officer and eventually progressed to Principal Research Officer and Section Head, Simulation and Digital Health at NRC. He currently oversees four biomedical software research teams that work in a variety of projects in collaboration with clinicians and industry. Projects his researchers have worked on range from the development of a surgical skills simulator, virtual-reality cognitive care and remote interactive patient management.
Invited Speakers
 Dr. Rob Power, EdD
Dr. Rob Power, EdD
President, Power Learning Solutions
President, International Association for Mobile Learning
Adjunct Professor of Educational Technology, Athabasca University, Cape Breton University, Mount Royal University, Ontario Tech University, University of Manitoba
Dr. Power will discuss opportunities to leverage mobile technologies for just-in-time learning for emergency health care professionals, and to improve communication with patients. Dr. Power will also identify some of the pitfalls with the use of mobile technologies in emergency patient care.
Rob Power is the President of Power Learning Solutions. He also teaches graduate-level educational technology courses in distributed learning contexts at 4 major universities. Dr. Power has taught information and communications technology at the K12 and post-secondary levels, and has worked as an instructional developer in the higher and continuing education sectors. Since 2013, he has taken a leading role with the International Association for Mobile Learning (IAmLearn), and has served as the Chair of the 12th World Conference on Mobile and Contextual Learning (mLearn 2013). Dr. Power was elected President of the Executive Committee of IAmLearn at mLearn 2017.
 Dr. Aikta Verma, MD MHSc FRCPC
Dr. Aikta Verma, MD MHSc FRCPC
Chief, Department of Emergency Services, Sunnybrook Health Sciences Centre
Assistant Professor, University of Toronto
Dr. Verma will be speaking about how they use physician iPhones at Sunnybrook Hospital to improve flow through the Emergency Department.
Dr. Aikta Verma is the Chief of the Department of Emergency Services at Sunnybrook Health Sciences Centre, a tertiary-care, academic hospital in Toronto. As the first woman in this position, she strives to address issues around bias, diversity, equity, and wellness. She completed a Master’s Degree in Health Administration, with a special interest in Quality Improvement, and she conducted groundbreaking research about push-alert notifications to ED physician smartphones. She is an Assistant Professor at the University of Toronto, and has held several leadership roles in the Emergency Medicine residency training program, including Assistant Program Director.
 Dr. John Pawlovich, MD FCFP
Dr. John Pawlovich, MD FCFP
Program Coordinator, REAP (Rural Education Action Plan, BC)
Medical Director, Carrier Sekani Family Services
Clinical Professor, Department of Family Practice, University of British Columbia
Sector Lead, Rural Coordination Center of BC (RCCbc)
Dr. Pawlovich will share his experience using simulation in the rural emergency room using virtual care technology
Dr. John Pawlovich is a Clinical Professor in the Department of Family Practice at University of British Columbia (UBC). He has worked in many rural and remote sites across Canada. Over the last twenty plus years, his interest in Indigenous Health has evolved with a focus of bringing innovative primary care and specialty services onto reserve to reach the people most in need. Using new technology such as telehealth from his home office in Abbotsford, British Columbia, Dr. Pawlovich is able to connect to multiple remote aboriginal communities to help provide the daily primary care they deserve and need.
Dr. Pawlovich is a co-founder and co-lead of the BC Virtual Health Grand Rounds and the e-Health theme lead for the UBC Faculty of Medicine. He speaks both nationally and internationally on virtual healthcare solutions and systems.
Presenters
Vincent Farquhar, RN BN MMEd
Faculty, Emergency Nursing Specialty, British Columbia Institute of Technology
Virtual Simulation Modalities to provide realistic situations for emergency nursing students
Specialty Nursing at the British Columbia Institute of Technology (BCIT), have developed a range of innovative virtual simulation modalities that enable emergency nursing students to actively apply the learnt curriculum in a novel, fun and realistic way. When designing a virtual simulation-based activity, we sometimes hear people say “yeah, but in the real world I would do this…”? How real do you get with AR/VR and screen-based simulation activities? In the world of specialty nursing students, realism is critical to meeting the learning outcomes of the program. In order to increase competence and confidence, specialty nursing students need to be exposed to a multitude of patient cases such as burn victims, gunshot wounds, traumatic head injuries, and other high-risk, low frequency cases. So, which simulation modality (AR/VR/ Screen-based) provides the most realism and is the most practical, in terms of design, development and delivery, for oncampus and distance students? Will off-the-shelf products meet the learning outcomes or do you develop a customized application?
We all have ideas on how to use innovations to improve patient care and health system transformation. But what does it take to make these ideas and products come to life? How do the different stakeholders work together to create and facilitate true and lasting impact?
This panel features 2 conference keynote speakers, Dr. Shez Partovi & Dr. Teresa Chan, as well as other experts in the healthcare innovation space, shown below, all of whom will help make sense of the diverse roles involved, and identify key steps to translate innovations to real-life practices.
 Darcia Pope, BComm MHA
Darcia Pope, BComm MHA
Vice President and Chief Transformation Officer, Vancouver Coastal Health
Darcia is Vice President and Chief Transformation Officer at VCH, where she oversees the strategic and operational planning processes, supports the measurement and realization of enterprise-wide strategic initiatives and leads the Innovation Portfolio. Darcia joined VCH in 2002 as Director of Enterprise Services in IMITS before moving into the new position of Executive Director of Transformation focusing on Workforce Optimization, Primary and Community Systems projects, and Strategic Initiatives. Prior to joining VCH, she held roles at St. Paul’s Hospital and was the Change Leader for the amalgamation of Providence Health Care.
 Dr. Ryan C.N. D’Arcy, EngL BSc MSc PhD
Dr. Ryan C.N. D’Arcy, EngL BSc MSc PhD
President and Chief Scientific Officer, HealthTech Connex, Inc.
Professor & BC Leadership Chair, Faculty of Applied Sciences, Simon Fraser University
Surrey Memorial Hospital Fdn. BC Leadership Chair in Multimodal Tech. for Healthcare Innovation
Head, Health Sciences and Innovation, Surrey Memorial Hospital
Dr. Ryan C.N. D’Arcy, EngL is neuroscientist and entrepreneur. He co-founded both the Health and Technology District and Health Tech Connex in BC. He is an Engineer Licensee in neurotechnology, and did his post-doctoral training in medical imaging physics at the National Research Council’s Institute for Biodiagnostics. He spent over a decade at the NRC, leading the development of Atlantic Canada’s biomedical imaging cluster. In 2012, he began developing BC’s health technology innovation cluster and continued translational neuroimaging and neurotechnology initiatives in point of care technologies, functional MRI, MEG, and EEG monitoring, and advanced multimodal neuroimaging R&D.
 Megan Stowe, RN BN MScN
Megan Stowe, RN BN MScN
Executive Director for Virtual Health and Clinical Education, Vancouver Coastal Health
Megan Stowe is the Executive Director for Virtual Health and Clinical Education at Vancouver Coastal Health Authority. Holding previous roles such as Chief Clinical Information Officer, Clinical Director of Redevelopment and Provincial Director of Operations Megan has become passionate about transformation in healthcare through the intersection of leadership, quality improvement, education and technology. Megan has previously led the implementation of electronic documentation and is currently leading Vancouver Coastal Health’s Virtual Health transformation.
 Dr. Damian Claydon-Platt, MBBS GradDip InfSys PhD CHIA MACHI AFRACMA CPHIMS-CA
Dr. Damian Claydon-Platt, MBBS GradDip InfSys PhD CHIA MACHI AFRACMA CPHIMS-CA
Chief Clinical Information Officer, IMITS VPP, VCH, PHSA, & PHC
Executive Lead, Clinical Systems + Transformation Project, CST
With 20 years of clinical experience in intensive care and 5 years as Chief Clinical Information Officer (CCIO) at large healthcare organizations, Damian Claydon-Platt is currently the Executive Lead of the Clinical Systems + Transformation project. In this role, he is working to improve the technology ecosystem within healthcare, to support improvements in safety, quality and efficiency, as well as positioning the project to take advantage of the numerous transformation opportunities presented by digitization. He is deeply passionate about the digital transformation of healthcare at all levels.
 Dr. Leanne Currie, RN PhD
Dr. Leanne Currie, RN PhD
Associate Professor, School of Nursing, University of British Columbia
Core Faculty, Designing for People Initiative, University of British Columbia
Co-Director, Research, Canadian Nursing Informatics Association
Core Faculty, Centre for Artificial Intelligence for Decision in Action, University of British Columbia
Dr. Leanne Currie is an Associate Professor at the University of British Columbia School of Nursing where she conducts research in the field of nursing, biomedical and health informatics. Her program of research focuses on clinicians’ use of technology to support their work including computerized clinical decision support systems, user-centred design methods, biomedical informatics education, and the impact of technology on clinicians’ work and patient outcomes.
More speakers and panelists will be announced closer to the conference. Check back to this page and follow us @TECVancouverBC on Twitter, Facebook, and Instagram to stay up-to-date.
FOAM Bar
At recent conferences in Emergency Medicine, it has become a common sight to have a Free Open Access Medical Education (FOAM) Bar. This is a resource for conference participants where they can get hands on tips and tricks to help them access blogs, apps, and podcasts to make the most of FOAM. During breaks or just on the way to get coffee, participants can interact with volunteers and use computers and mobile devices to see common use of social media and the internet to access medical resources.
Make sure to check out the FOAM Bar at TEC Vancouver - it will be available for all attendees to visit during breaks between sessions. Many thanks to the staff of the Department of Emergency Medicine at Vancouver General Hospital for providing this fantastic resource!
Organizers
Digital Emergency Medicine is a research unit in the UBC Faculty of Medicine Department of Emergency Medicine, with the goal of introducing, researching and implementing technology innovations in emergency and primary care with their interdisciplinary partners to improve people’s health and strengthen health systems.
The Department of Emergency Medicine at Vancouver General Hospital (VGH) sees over 95,000 patients per year and houses a Level 1 Trauma Centre. VGH is a 955 bed adult tertiary care hospital focusing on tertiary, trauma, and neurological care. The Emergency Medicine group at VGH supports strong research and academic educational programs.
The VGH + UBC Hospital Foundation is the philanthropic engine for health care innovation and transformation in British Columbia. As the primary philanthropic partner to Vancouver Coastal Health (VCH) — BC’s largest health authority — the Foundation partners with donors to drive innovation and sustainable health care at Vancouver General Hospital (VGH), UBC Hospital, GF Strong Rehab Centre, Vancouver Coastal Health Research Institute (VCH Research Institute), and Vancouver Community Health Services.
Vancouver Coastal Health Authority (VCH) is a world class, award winning health care organization delivering innovative medical care, research and teaching. It provides primary through quaternary care, home and community care, mental health and substance use services, as well as population and preventive health to over 1.25 million British Columbians.
Thank You to our Sponsors
Platinum Conference Sponsors
Connect with Us
Twitter: @TECVancouverBC | Facebook: @TECVancouverBC | Instagram: @TECVancouverBC